Our research and personalized medicine
Everyone is unique!
So why do psychiatric treatments still rely on a one-size-fits-all model? Our main motivation and the core of our research revolves around the topic of ‘personalized medicine’. We move beyond traditional ‘diagnostic-thinking’ and focus on individual differences that can help optimize and individualize treatment or prevention strategies. To achieve this goal, our research focuses on multiple specialties listed below.
Neuromodulation
Neuromodulation describes a family of new treatments in psychiatry. It aims to modulate brain activity directly and focally, through electrical stimulation (e.g. tDCS, tACS) and transcranial magnetic stimulation (rTMS) or via endogenous techniques like neurofeedback or psychotherapy. Opposed to pharmacological approaches that rely on systemic application of psychoactive drugs, neuromodulation relies on neuroplasticity. It offers a new window of opportunity to change and modulate brain activity. For more detailed reviews and scientific backgrounds, see Neurofeedback in ADHD and rTMS in depression
For interested clients seeking neuromodulation treatment also see the neuroCare Clinics website
Heart-Brain Coupling
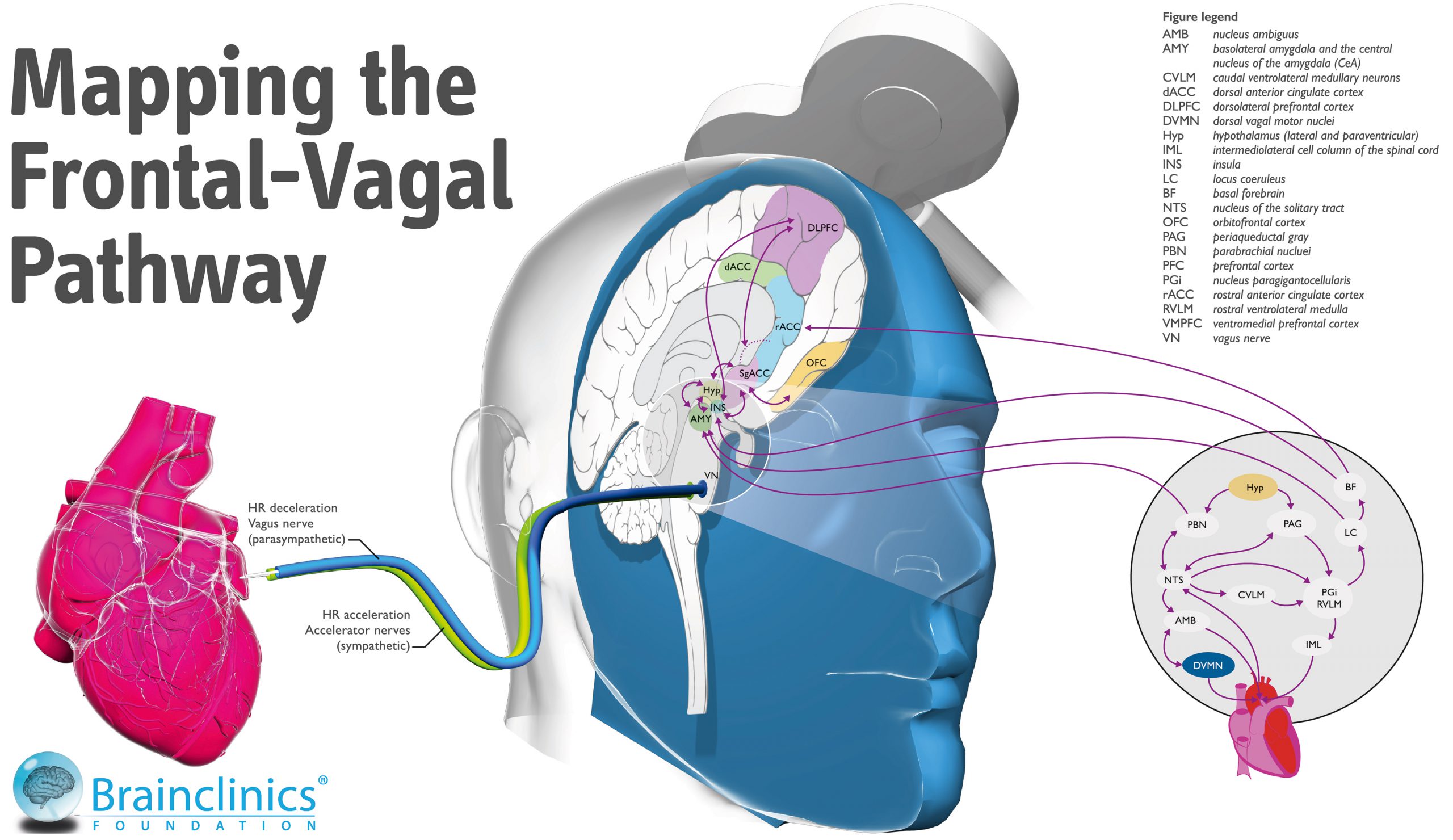
One specific example where we pioneered a more individualized approach to rTMS in the treatment of depression is through Neuro-Cardiac-Guided TMS, or Heart-Brain Coupling.
Applied Neuroscience
The broad field of ‘neuroscience’ currently comprises close to 400.000 scientific studies as indexed in PubMed. Most of these studies are relatively ‘fundamental’ studies, important in knowledge discovery, but failing to answer the ‘so what?’ question.
We specialize in ‘Applied Neuroscience’ with a focus on advancing neuroscience from the lab to the clinic, so it can more quickly and directly serve the people that need it most.
Biomarkers and Stratified Psychiatry
An important biomarker technique we use is Electroencephalography (EEG), either Quantitative EEG (QEEG) or Event Related Potentials (ERP’s). For further background reading, see history from EEG to QEEG, the EEG as a biomarker or endophenotype, and some EEG examples of subtypes like a Low-Voltage EEG and Beta spindles.
The application of these biomarkers is a crucial development on the path to personalized medicine and stratified psychiatry, and one of the cornerstones in our research efforts, also see our stratified psychiatry page.
The Heart-Brain Coupling app for iOS
The Brainclinics Foundation developed Heart-Brain Connect, a breakthrough Heart-Brain Coupling app to assist clinicians in pinpointing the optimal location for rTMS treatment. Our unique approach has great advantages over more traditional methods and can be tried for free. The app can also be used as a resonant breathing training method.
For more information, please visit this page.
Heart-Brain Connect is available in the iOS App store.
Personalized Insights
An example of new personalized insights is our neuroscience research in ADHD. We investigated excess theta EEG activity as a biomarker in ADHD, and linking this biomarker to sleep we began to understand the role of the circadian system better. We eventually proposed and tested a theory that shed further light on the role of sleep in the etiology of ADHD. Below, use the slider to see one of our primary findings. It demonstrates the overlap between the prevalence of ADHD (blue) and the intensity of sunlight (orange and yellow). It clearly suggests a preventive effect of sunlight in developing ADHD mediated by the circadian system, or biological clock (Arns et al., 2013; Biol. Psychiatry). For an easy to read summary see ADHD, sleep and tablets or in Dutch, follow this link ADHD, slaap en tablets: een ander licht op ADHD.
The association between ADHD prevalence (blue) and sunlight intensity (orange-red), mediated by the sunlights capability to synchronize the biological clock. Use the slider to see the clear overlap.
Clinical Trials
We are involved in several clinical trials and multicentre studies, and only take part in clinical trials that are close to our mission and vision.
TETRO-Trial: Combined CBT and rTMS in the treatment of OCD
The TETRO trial is a multicenter randomized RCT, where 250 patients with OCD will be randomized to Cognitive Behavioral Therapy (CBT) combined with real or sham rTMS aimed at the Supplementary Motor Area (SMA).
 iSPOT study in ADHD and Depression
iSPOT study in ADHD and Depression
We’re involved with the International Study to Predict Optimized Treatment in ADHD (iSPOT-A) and Depression (iSPOT-D) since 2008, a study sponsored by Brainresource. It’s the largest biomarker study worldwide,(20 clinical sites across the globe with 1008 recruited patients (depression), 332 patients with ADHD and 500 controls). Data collected before and after treatment (antidepressants or psychostimulant medication) included EEG, ERP, neuropsychological, clinical, imaging and genetics data . For published studies on this trial see our publications.
International Collaborative Neurofeedback Study (ICAN)
The ICAN Study is a NIMH (National Institute of Mental Health) funded study investigating the efficacy of neurofeedback for children age 7-10. It’s the first multicenter double-blind placebo controlled study on the efficacy of neurofeedback in ADHD in a sample of 140 children. The cross-site investigation team was selected for balance between neurofeedback and mainstream ADHD investigators, and for expertise in treatment strategy, assessment, design, biostatistics, data management, and multisite RCT execution.
Research, publications and education
For an overview of scientific publications, book chapters, books and media appearances by Brainclinics staff visit our Publications- or Media section
Have a look at an interactive model of the brain, or visit this page with downloadable research resources.
